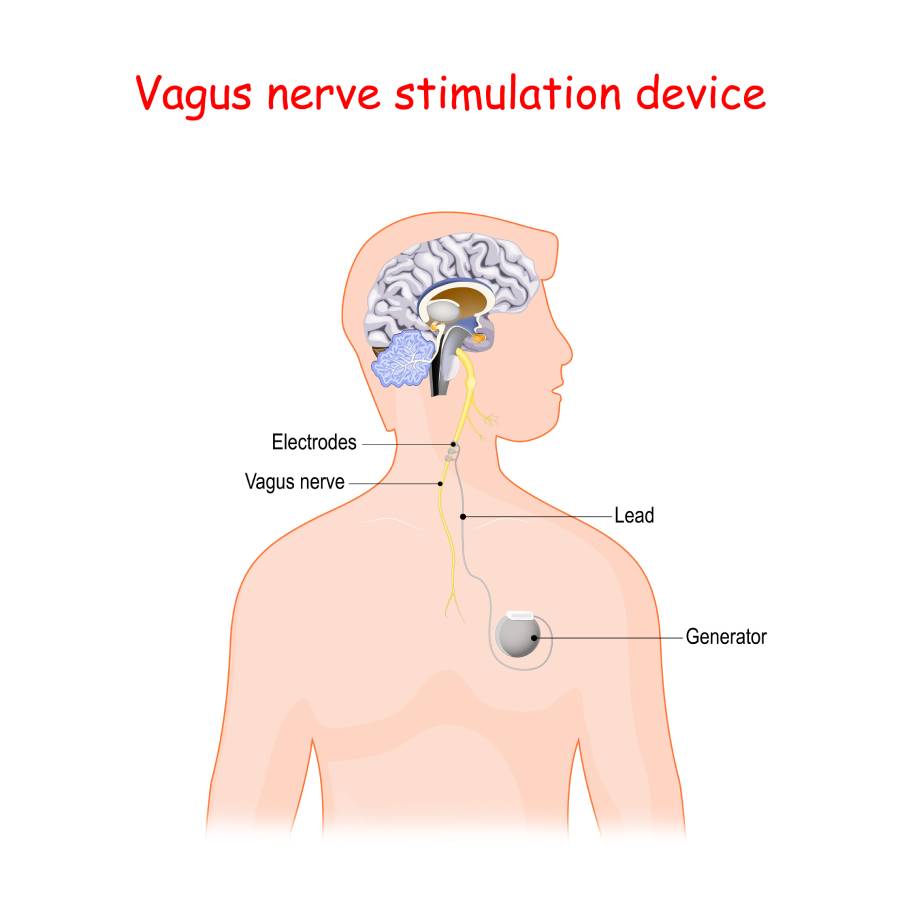
Vagus nerve stimulators are implantable neuromodulation devices primarily used for treating refractory epilepsy and treatment-resistant depression. As their uses expand, anesthesiologists are increasingly likely to encounter patients with these devices in the perioperative setting. A vagus nerve stimulator system consists of a pulse generator implanted in the chest wall with leads wrapped around the vagus nerve, typically below the carotid bifurcation. The device generates electrical impulses that modulate afferent vagal pathways, reducing seizure frequency and severity. However, the effects of the vagus nerve stimulator on the cardiovascular, respiratory, and autonomic systems impact anesthesia management when patients with these devices require surgery (1).
Perioperative management of patients with an implanted vagus nerve stimulator begins with a thorough preoperative evaluation. Healthcare providers should review the device’s function, indication, and stimulation settings, ideally in collaboration with the patient’s neurologist. Because VNS therapy can influence autonomic tone, patients may exhibit bradycardia or asystole during stimulation. There have been reports of intraoperative bradyarrhythmias, particularly during lead manipulation or generator activation (2). Therefore, the anesthesia plan for patients with vagus nerve stimulators must include continuous electrocardiographic monitoring and readiness to promptly intervene with anticholinergic or sympathomimetic agents if significant bradycardia occurs.
Effective communication between the anesthesia and surgical teams is essential during the perioperative period. Using a device designed to temporarily inhibit or activate stimulation provides a valuable safety measure. In order to minimize interference with cardiac and respiratory function, it is generally recommended that the device be deactivated prior to induction and remain off until the patient has recovered from anesthesia (3). However, this decision should be made on a case-by-case basis, especially for patients with intractable epilepsy, as abrupt cessation of stimulation may increase seizure risk.
Anesthetic agents themselves may influence seizure threshold and autonomic function, necessitating careful selection. Volatile agents, such as sevoflurane and desflurane, are generally safe. However, hyperventilation and hypoxia should be avoided, as they may provoke seizures. Propofol, which is widely used for induction and maintenance, is often preferred due to its anticonvulsant properties. In contrast, ketamine, which can lower the seizure threshold, is typically avoided. Opioids should be used cautiously, as they can have an additive effect on respiratory depression. This effect may be exacerbated by vagal nerve stimulation-induced laryngeal muscle stimulation and resultant airway obstruction (4).
Intraoperative monitoring should include vigilance for changes in respiratory mechanics. Stimulator activation may result in transient coughing, voice changes, or airway obstruction due to stimulation of the recurrent laryngeal nerve. Furthermore, vagus nerve stimulation therapy has been linked to the onset or worsening of obstructive sleep apnea (OSA) (5). Continuous pulse oximetry and capnography are recommended during emergence and recovery. Postoperatively, patients with OSA or other respiratory vulnerabilities should be monitored in a high-dependency unit until they have made a full recovery and the stimulator has been reactivated.
Electrocautery presents another unique challenge. Monopolar diathermy can induce current conduction through the system, which can lead to thermal injury to neural tissue or generator malfunction. To mitigate this risk, bipolar cautery should be used whenever possible, and the current path should be kept away from the generator and leads (1). If monopolar cautery is unavoidable, the grounding pad should be positioned to ensure the current does not traverse the device.
The presence of a vagus nerve stimulator adds complexity to perioperative management of anesthesia. Key considerations include preoperative verification of device function, intraoperative monitoring for autonomic instability, prevention of electrical interference, and postoperative respiratory vigilance. Close interdisciplinary coordination among anesthesiologists, neurologists, and surgeons ensures safe and effective care for this growing patient population.
References
- Broderick L, Tuohy G, Solymos O, et al. Management of vagus nerve stimulation therapy in the peri-operative period: Guidelines from the Association of Anaesthetists: Guidelines from the Association of Anaesthetists. Anaesthesia. 2023;78(6):747-757. doi:10.1111/anae.16012
- Giordano F, Zicca A, Barba C, Guerrini R, Genitori L. Vagus nerve stimulation: Surgical technique of implantation and revision and related morbidity. Epilepsia. 2017;58 Suppl 1:85-90. doi:10.1111/epi.13678
- Yamagata K, Hirose Y, Tanaka K, et al. Anesthetic Management of a Patient With a Vagal Nerve Stimulator. Anesth Prog. 2020;67(1):16-22. doi:10.2344/anpr-66-03-02
- Fahy BG. Intraoperative and perioperative complications with a vagus nerve stimulation device. J Clin Anesth. 2010;22(3):213-222. doi:10.1016/j.jclinane.2009.10.002
- Hatton KW, McLarney JT, Pittman T, Fahy BG. Vagal nerve stimulation: overview and implications for anesthesiologists. Anesth Analg. 2006;103(5):1241-1249. doi:10.1213/01.ane.0000244532.71743.c6